Smarter QA. Stronger Teams. Scalable Performance.
Better Patient Interactions Start Here
Your agents navigate Epic, Salesforce, and five other systems before lunch. AmplifAI unifies performance data across your entire tech stack—so supervisors stop scrubbing spreadsheets and start coaching the behaviors that drive patient satisfaction, appointment conversion, and regulatory compliance.

Powering the best in CX



COMPILANCE & CERTIFICATIONS




CHALLENGES
Top CX Challenges in Healthcare
Systemic CX challenges that create compliance blind spots, manual overhead, and inconsistent patient experiences across healthcare contact centers.
Fragmented Data Across EMR and CCaaS
Your telephony lives in one system. Patient records live in another. Supervisors spend 500+ hours scrubbing cases manually because the data never connects.
Manual QA Leaves Compliance Gaps
You're required to read Mini Miranda disclosures, verify co-pays, and document consent—on every call. Manual QA covers 3-5%. The other 95% is a compliance blind spot.
Empathy Can't Be Measured Manually
Agents follow the script but miss the moment. Measuring "care factor" in sensitive medical conversations requires more than a checkbox on a QA form.
Use Cases
Top Use Cases for AmplifAI in Healthcare
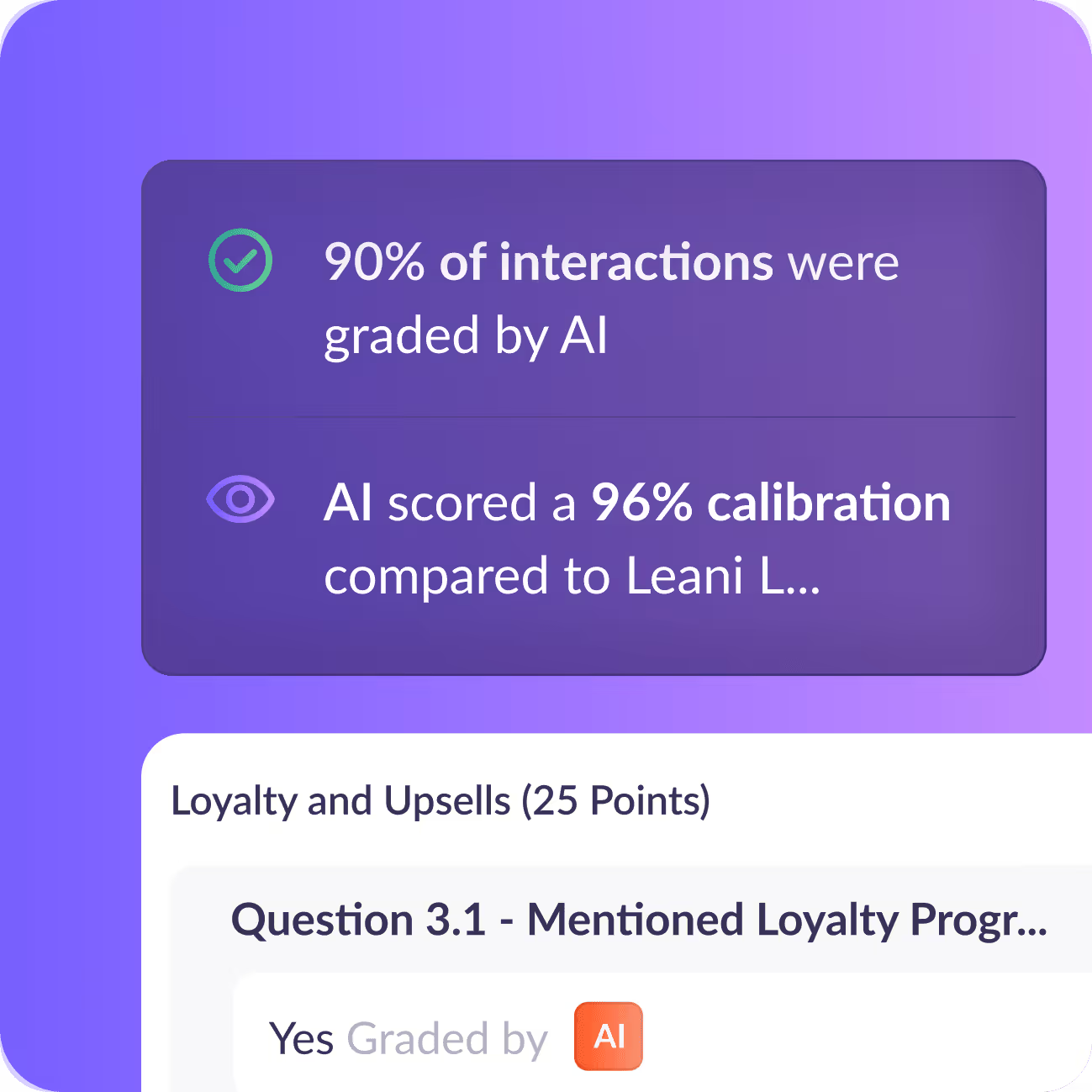
100% Automated Compliance Monitoring
CMS and HIPAA don't accept sampling. AmplifAI's Auto QA evaluates every interaction—calls, chats, emails—against your compliance criteria. Did the agent read the disclosure? Verify the co-pay? Document consent? The platform catches it, flags it, and creates an audit-ready trail. QA analysts shift from random sampling to targeted coaching on the violations that matter.
of interactions are reviewed by manual QA in healthcare contact centers—leaving 95%+ of compliance risk unmonitored.
Patient Access and Appointment Conversion
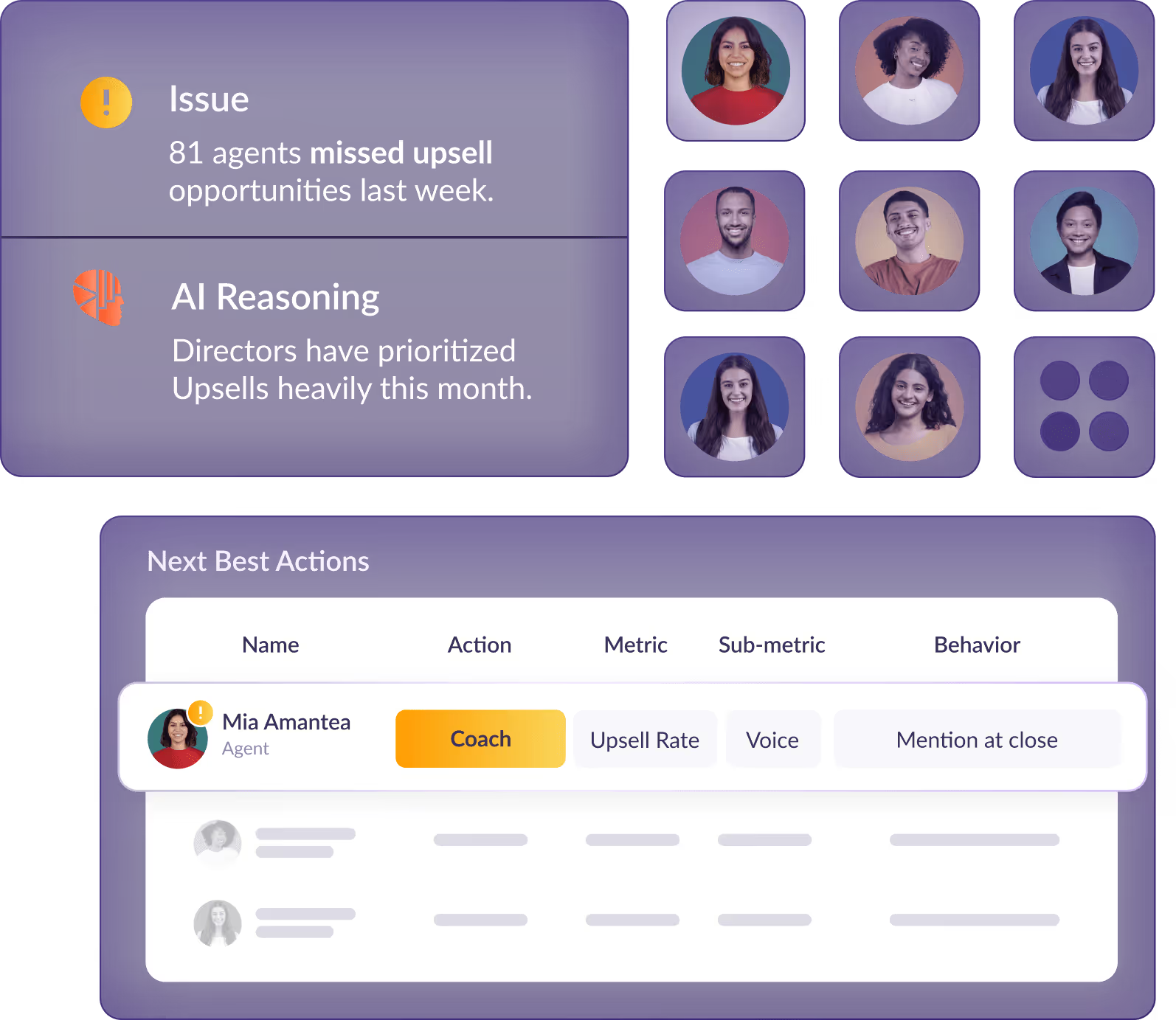
Every inbound call is a potential patient. AmplifAI surfaces the behaviors that convert inquiries into booked appointments—and the gaps that lose them. Supervisors see which agents struggle with objection handling, which scripts underperform, and where follow-up falls through. More conversions. More patients in chairs. More revenue captured.
increase in new patient appointments after implementing AI-driven performance coaching.
Empathy and Soft Skills at Scale
Patients remember how they were treated, not just what was said. AmplifAI measures empathy, active listening, and care factor across every interaction—not just the 5% your QA team samples. Supervisors get next-best-action coaching recommendations that address soft skill gaps before they become patient complaints or CAHPS score drops.
increase in coaching effectiveness when supervisors receive AI-driven recommendations on who to coach and what to coach on.
Customer Use cases
Success stories from healthcare organizations
How healthcare BPOs turn AI insights into compliant, scalable, and measurable CX outcomes.


AmplifAI helped University of Miami Health System increase appointments and conversions by 34%
AmplifAI helped University of Miami Health System increase appointments and conversions by 34%


Overview
Patients hate waiting for their appointments.
The University of Miami Health System delivers leading-edge patient care by the region’s best doctors, powered by the groundbreaking research of the University of Miami Leonard M. Miller School of Medicine. As South Florida’s only university-based medical system, UHealth is a vital component of the community that is leading the next generation of health care.
UHealth is made up of more than 1,200 physicians and scientists who are highly trained specialists focused on providing state-of-the-art medical care. From diagnosis to treatment and follow-up, physicians work in teams to tailored care to each patient.
Patients from around the world turn to UHealth - University of Miami Health System in their search for expert care from our top ranked physicians. UHealth is home to the number one eye hospital in the United States, Bascom Palmer Eye Institute, the only NCI-designated cancer center in South Florida, Sylvester Comprehensive Cancer Center, a pioneering minimally invasive cardiac surgery program, and offers expertise in more than 100 medical specialties. UHealth’s comprehensive network also includes more than 30 sites.
International patients come for consultations with our renowned physicians, advanced treatment technologies, leading-edge medical therapies, and state-of-the-art surgical procedures. Whatever your reason for coming to UHealth International, you receive customized medical care delivered within a compassionate, multicultural setting.
A leading South Florida hospital system was experiencing growth in both ambulatory and acute care visits, spending more than $2.5M per year on mass patient communication and appointment setting systems. The communication systems in place were developed 10+ years ago and not designed to handle today’s 1200+ providers and their respective patient network. The belief was that the spend was excessive for an antiquated system and had many gaps based on competitive research; median call abandonment rate of 19.2%, an average speed of answer of 2 mins and 49 seconds, high number of no-shows and multi-channel communication expectations. As one of the top hospital systems in the country, they recognized the need to examine their contact center to ensure better communication with patients and providers.
Pain Points
- Patients demanded better experience and service.
- Services and appointments were being rescheduled, creating empty slots.
- Handle time was taking too long to reach a resolution.
After assessing the organization and identifying the characteristics of the contact agent population, we established data pipelines to various source systems.
Solutions
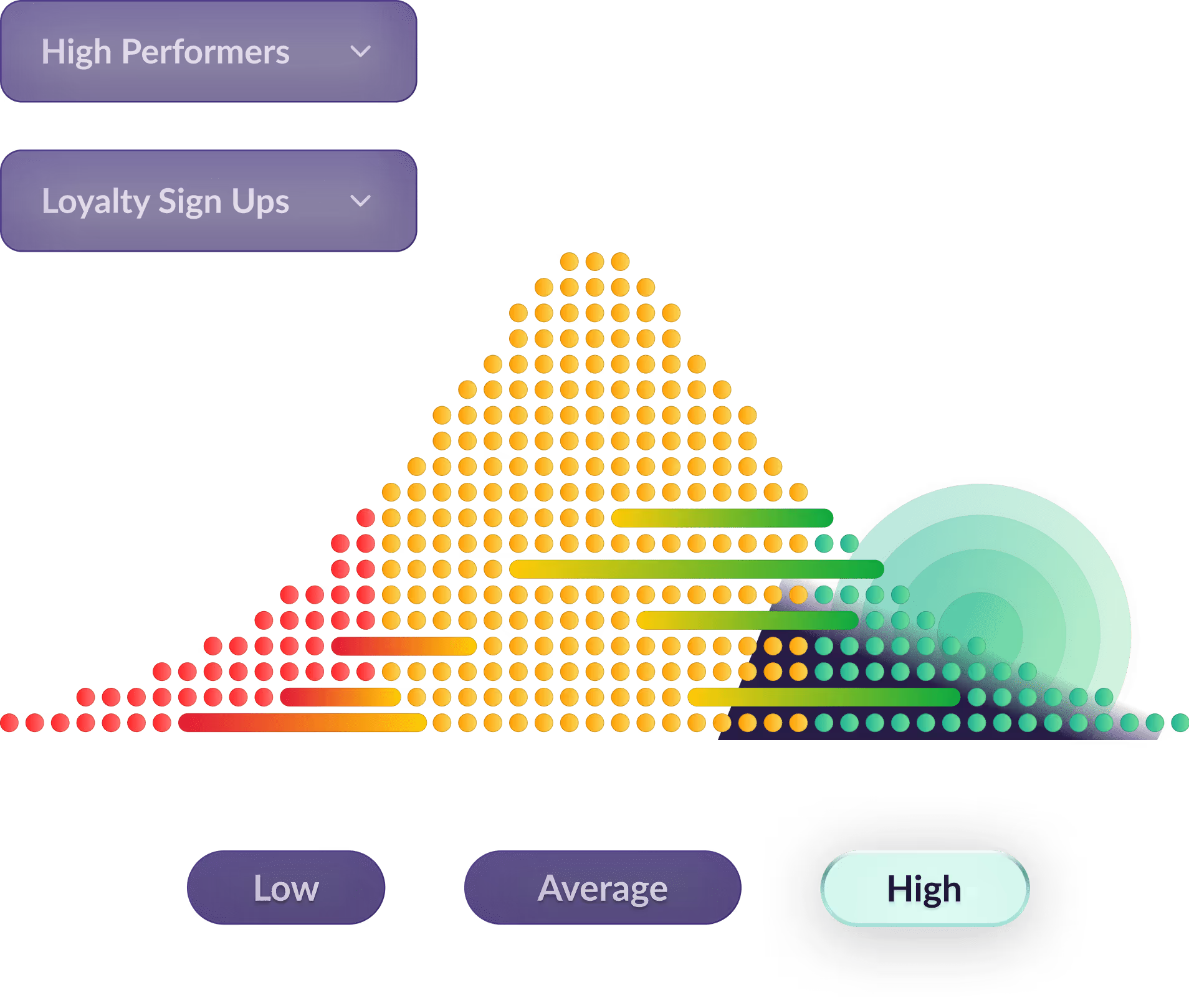
We provided a 3-tier dashboard view (contact agents, frontline managers and executives) so actions can be specific to the user’s role and area of responsibility. By continuing to push the distribution of the population towards high-performers, we were able to see noticeable improvement in better forecasting and scheduling of patients. In addition, the patients’ experience and journey showed significant improvement towards the previous months.
AmplifAI provided us with an intelligent platform that simplified our data and reports from various systems into easy to understand views and recommended detailed actions to engage and develop agents across our scorecard. AmplifAI allowed us to engage, develop and communicate effectively with our workforce both remote and on-site while making coaching and learning focused, effective and fun.
Cary Danner, Assistant Vice President UHealth Connect
.png)

SSM Health decreased write-offs by 55% in only 3 months
SSM Health decreased write-offs by 55% in only 3 months

.png)
Opportunity
In order to meet the high expectations and standards of the healthcare industries and health systems, AmplifAI was utilized to improve coaching effectiveness and improve associate performance. They utilized:
- AI-powered tasks, coaching & recognition bots
- Smart data and knowledge processing
- Intelligent contact center solution empowering digital labor
Previous Pain Points
- Manual assessment of reports and metrics reduced coaching time
- Client was disappointed when patients did not pay their balance
- Measuring and action on productivity was delayed especially with WFH
Monthly write-offs decrease over first three months

“AmplifAI helped us solve for so many issues as we transitioned to a remote workforce. Our leaders had clear actions prioritized to business needs and our associates had easy access to their performance data and actions along with connections to best practices. This was a complete transformation of our operation that improved productivity and performance resulting in a much more significant ROI than expected.”
Chief Admin Officer, SSM Health



Global healthcare business process leader improves retention by 12%
Global healthcare business process leader improves retention by 12%


About the Client
This global healthcare business process management leader combines domain expertise with technology powered services to serve leading providers and payers.
The organization was particularly interested in managing associate performance across client teams serving three different major healthcare payers in Member Services, Provider Services, and Enrollment.
The Opportunity
The healthcare business faced a low level of engagement in their frontline associates and a high attrition rate above 11% a month.
This high cost of attrition amounted to about 2.5x the monthly compensation of anAssociate. This meant the opportunity for improvement was significant in both operational and financial terms.
Overall, the global healthcare BPO wanted to,
- Increase the engagement level of associates
- Improve the attrition rate of associates
- Reduce the annual cost of attrition
Solution and Impact
The client implemented AmplifAI's performance enablement solution with a focus on helping improve associate engagement, coaching effectiveness, and employee recognition.
AmplifAI became the one system to see and understand all the healthcare organization's performance data relative to their goals. The platform also provided system-generated intelligent coaching and recognition actions for both supervisors and agents.

In just three months, the business process leader realized a 12% improvement in the retention rate of the associates serving their three major payer clients. The attrition rate declined from 11.1% in October to 9.8% in December.
The financial benefit of this attrition reduction is estimated to be in excess of $1,500,000 each year.
Frequently Asked Questions
Learn how AmplifAI helps healthcare organizations improve compliance, elevate patient experience, and run high-performing contact centers with less manual effort.
How do you handle PHI/PII and HIPAA compliance?
AmplifAI is HIPAA compliant and SOC 2 Type II certified. We support multiple data handling approaches: you can redact transcripts before sending, or we can redact upon ingestion. Sensitive patient data never needs to leave your environment if your policies require it.
Do you integrate with Epic and other EMRs?
Yes. We integrate with Epic, Cerner, and other EMR systems—typically via reports or data exports. Humana was the first in their space to roll out Epic integration with AmplifAI. We pull the performance data you need without requiring deep bi-directional system access.
Can you transcribe audio, or do we need to send transcripts?
Both. AmplifAI can ingest your existing transcripts or transcribe audio directly. For organizations with legacy on-prem systems (Avaya, Cisco), we're flexible—send us what you have. If we transcribe, you control whether redaction happens on your end or ours.
Can you distinguish between different lines of business (Medicare vs. Commercial)?
Yes. The platform hierarchy supports separate scorecards, QA forms, and metrics by line of business. Your Medicare team can have different compliance criteria than Commercial—each with its own dashboards, benchmarks, and coaching workflows.
Does the AI understand medical terminology?
Yes. We prime the model with your specific content—plan documents, clinical glossaries, product guides—so it understands your terminology in context. When the AI evaluates whether an agent "correctly quoted the co-pay," it knows what correct looks like for your organization.
Interact with self-service demo
See how healthcare organizations unify EMR and CCaaS data, automate compliance monitoring, and coach for patient satisfaction.
Talk to sales
AmplifAI your CX
30 minutes today can extend your contact center capacity by 30%.